The temporomandibular joint, or the jaw, is one of the most commonly under-treated regions in the body and can contribute to significant head, neck and facial pain. Some research suggests that one half of the population will experience one symptom of temporomandibular joint dysfunction in their life, but only 3.5-7% of those will actually seek treatment. Below are frequently asked questions about temporomandibular joint dysfunction and how physical therapy can be beneficial.
What is the temporomandibular joint?
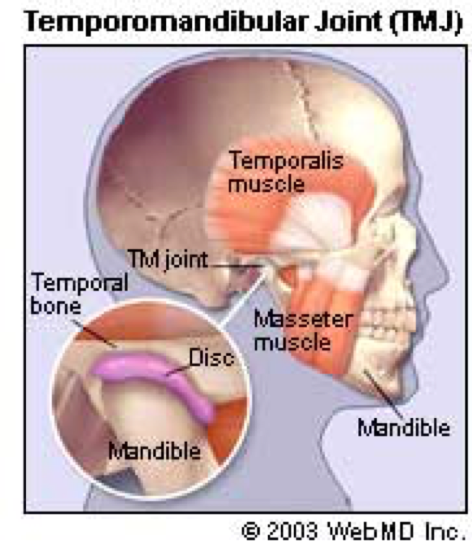
The temporomandibular joint, or TMJ, is a pair of joints located on the sides of the face, just in front of the ears, where the jaw bone (mandible) attaches into the skull (temporal). These joints assist with chewing and speech and can become dysfunctional resulting in limited function and pain. Related to the bones are the muscles that act across the joint, disks, ligaments, and joint capsules that can contribute to the pain and dysfunction.
What is temporomandibular dysfunction?
Temporomandibular dysfunction, or TMD, is a collective term for symptoms related to the cranio-facial-mandibular complex defined by worsening symptoms related to chewing and jaw movements independent of local disease involving the mouth or teeth.
Symptoms commonly described are:
- Pain in the jaw, face and side of the head
- Limited jaw function, including stiffness, pain with chewing, limited opening
- Headaches, neck pain
- Dizziness, ear pain, and tinnitus (ringing in the ears)
The nerve supply of the joint and surrounding tissue has significant overlap with the upper neck region, face, and head, which can help to describe why the TMJ can be present with a wide-array of symptoms. This also presents an opportunity for physical therapists to treat the TMJ and make a significant improvements in pain and function with chewing and speaking.
Common sources of pain and dysfunction are:
- Articular surface degeneration (Osteoarthritis, Rheumatoid arthritis).
- Disk displacement with or without reduction (clicking, locking).
- Trauma resulting in fractures, dislocations.
- Myofascial pain secondary to strains and trigger points.
- Cervical spine and posture dysfunction leading to poor body mechanics and altered nervous system input.
How can physical therapy help?
Physical therapy has been involved in the treatment of TMD over the past 50 years and a wide body of research demonstrates that the addition of physical therapy to management of TMD to be beneficial. Physical therapy interventions may include joint mobilizations and dry needling, postural education, neck mobility and strengthening, and activity modifications. Proper examination and assessment is crucial in determining how to best address TMD as well as identifying an appropriate referral to a dental professional if there are other contributing factors outside of the scope of physical therapy.
If you have been experiencing any of the symptoms we mentioned in this post, give our office a call. Our therapists are here to help! In the meantime, we have included some helpful videos below.
Cervical retractions
Jaw relaxation
Self-massage for Masseter